Living with

“We thought, ‘Okay, I can breathe. We’re going to try to do everything we can to deal with this disease.’”
Patricia, living with advanced melanoma & Byron, her caregiver
What is advanced melanoma?
Melanoma is diagnosed based on stage: I, II, III, or IV. Advanced melanoma is melanoma with metastasis (Stage IV, also called metastatic melanoma) or unresectable Stage III melanoma.
Stage IV melanoma is also known as metastatic melanoma and may or may not have spread to lymph nodes. Most patients diagnosed as Stage IV have unresectable melanoma.
- If you have Stage IV melanoma, your care team will consider location of the metastases, the number and size of tumors, as well as
lactate dehydrogenase (LDH)levels. - You may see a letter after an “M1”. The letter tells your care team where the metastases (“M”) are in your body. The number one means there is metastasis, as is the case for all Stage IV melanoma.
- M1a means it has only spread to
distantskin, other tissue such as muscle, and/or distant lymph nodes - M1b means the tumor had spread to the lungs
- M1c means tumor spread to internal organs, not including brain and/or spinal cord
- M1d means it spread to the brain and/or spinal cord
- M1a means it has only spread to
Stage III melanoma has not spread to distant parts of the body (no metastasis) but may have spread to nearby lymph nodes.
- There are subgroups of Stage III melanoma: IIIa, IIIb, IIIc, IIId. Your care team knows how to determine this based on tumor size and which lymph nodes are affected.
- Some Stage III melanomas may be completely removed with surgery (resectable).
UnresectableStage III melanoma cannot be completely removed with surgery and may be treated similarly to Stage IV.
Advanced melanoma may be your first diagnosis, or it can happen later on, if an earlier stage spreads. It is common to feel sadness, grief, fear, guilt, loneliness, fatigue, or pain.
Watch and Learn More About Mary and Jeff’s Path with Advanced Melanoma
Your Path
Know Where You May Go
Each body is different, and everybody reacts differently to each therapy. Advanced melanoma is complicated. It is important to be educated, stay informed, and keep in contact with your doctor as you develop a path forward.
Your treatment path or plan maps out the next steps for you.
- Surgery may be an option to remove the original tumor or lymph nodes for resectable disease. If eligible, patients may also have
neoadjuvantand/oradjuvant therapy. Systemic therapyis often recommended for patients with advanced melanoma. In advanced melanoma, initial therapy can be calledfirst-line, and the following treatmentsecond-linetherapy.Immunotherapyis the most common first-line therapy for advanced melanoma (about 62% of patients1,*), more specifically, a regimen that includes one or moreimmune checkpoint inhibitors(a type of immunotherapy that targets specific “checkpoints” in your immune system).Targeted therapieshave also improved lives for patients with specific gene changes such as BRAF, MEK, and KIT. About half of patients with melanoma have a BRAF mutation.†- The first approved treatment for advanced melanoma was a
chemotherapymedicine called dacarbazine and is sometimes still used for some patients with advanced melanoma.

“I brushed all of these thoughts and feelings aside, knowing the most important thing to do in the moment was figure out my next steps.”
Hillary, living with advanced melanoma
Watch to Learn More About Hillary’s Path with Advanced Melanoma
Evolution of Therapies for Advanced Melanoma
The following picture demonstrates how the number of available therapy options for patients with advanced melanoma has grown over time. It can also help organize the types of therapies, shown based on the years they became available in the US.
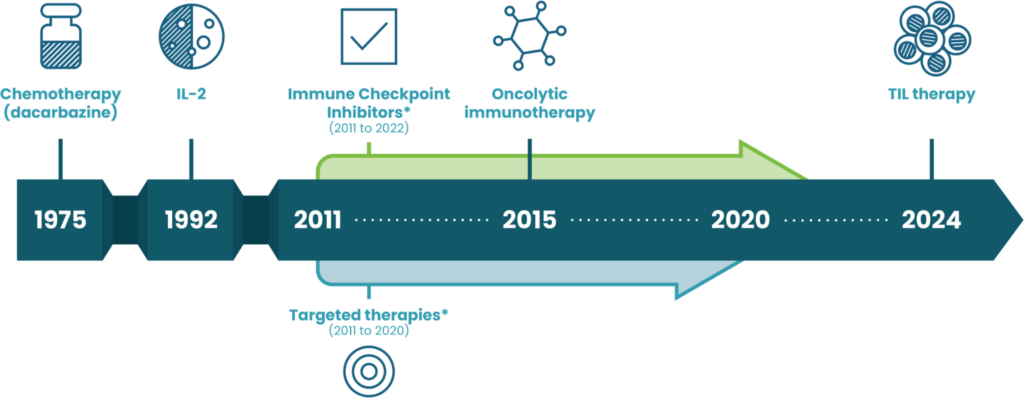
TIL=tumor infiltrating lymphocyte
*The areas shown represent many kinds of therapies that were introduced during this time period.
While not shown, there are also many types of therapies in clinical trials that may be available for patients with advanced melanoma who progress on current therapies.
WHAT’S AFTER
PROGRESSION?
Be Prepared for What is Next
Progression occurs for most patients taking therapy for advanced melanoma, even if it may have worked for a period of time. Your care team will monitor for progression during any line of therapy with special tests, including surveillance imaging such as computed tomography (CT) scans or magnetic resonance imaging (MRI).
The time it takes to experience progression cannot be easily predicted for each patient, and estimates vary depending on many factors such as the person being treated and the type of first-line immune checkpoint inhibitor regimen used for patients with advanced melanoma.
Up to 65% of patients with advanced melanoma may experience progression on immune checkpoint inhibitor(s) and may not know of other options available to them.2,3,4,‡
And some patients (up to 36%) are still responding to treatment or have not had tumor growth after 5 years.2,3,‡

“I just decided that I was going to roll up my sleeves, back into a corner and fight with everything that I have.”
Patricia, living with advanced melanoma
Hope After Progression
It is important to be prepared and understand your options for the next step in your treatment path. Talk to your doctor to learn more.
Feel empowered to talk with your care team about your potential options after progression
Discover Patricia and Byron’s Journey with Advanced Melanoma
Speak Up and
Ask Questions
You can try to be one step ahead of advanced melanoma. Whether you are living with advanced melanoma, or someone you love has advanced melanoma, there are ways to take an active role in care.
Planning ahead may help better prepare everyone for the future, including:
- Mapping out a possible treatment path with your healthcare team
- Managing expectations on what to expect
- Staying up-to-date on advanced melanoma research
- Knowing how to help yourself or others within your advanced melanoma community
Expand Your
Community
Make Your Own Path with a Community of Support
Whether you are living with advanced melanoma, or care about someone who is living with advanced melanoma, building and connecting with your own community of support can provide:
- inspiration from others with advanced melanoma
- tips for self-care and coping with overwhelming feelings
- education for planning future treatments
- the latest research on advanced melanoma
- a social network of others who understand

“Find a community and reach out to people that have gone through similar situations, but also know that you can reach out to your doctors.”
Hillary, living with advanced melanoma
Here are a few advocacy groups that may help you build and connect with a community:
Melanoma Research Foundation (MRF)The MRF is dedicated to advancing melanoma research, providing education, and supporting patients.
Melanoma Research Alliance (MRA)The MRA focuses on accelerating medical research and advancing treatments for melanoma, aiming to enhance understanding and find cures for aggressive skin cancer.
AIM at Melanoma FoundationAIM at Melanoma is committed to increasing awareness of melanoma and funding research for better treatments. It offers educational resources and support for patients and their families.
Cancer Support Community (CSC)The CSC provides emotional support, education, and resources for cancer patients and their families. It offers programs that focus on wellness, emotional health, and coping strategies.
American Cancer Society (ACS): Caregivers and FamilyThe ACS supports caregivers and families affected by cancer through education, resources, and community programs that offer guidance on navigating the cancer journey.
There are many words that you may hear from your care team, or while searching online. If you need help to better understand them, the National Cancer Institute (NCI) has a Dictionary of Cancer Terms that can quickly define complex words.
Stay Connected
Follow us on Facebook and Instagram or sign up for inspiring stories, the latest updates, and support. Join our community today!
KNOW THE
QUESTIONS
TO ASK
Life is not simple. Advanced melanoma is not simple. Educate yourself.
While your care team understands management options and can help you make decisions, you know your body best. Help your care team and loved ones understand how you feel, what you need, what is working or not working, and your goals to make shared decisions.
You are the most important part of your care team. It is important you know when you need more information and that you feel comfortable asking questions to your care team.
The following questions were co-created with the Replimune Patient Steering Committee, a group of patients and caregivers impacted by advanced melanoma.
It is important to be ready and plan ahead before progression to know your possible options. Stay motivated to educate yourself and loved ones on what you learn, to speak up and bring questions to your care team.
Each option has a different way that they work and may even have different ways they are given to your body.
Clinical trials may also be a consideration. Talk to your care team if you’d like to learn more.
Building and connecting with your own community of support may give you inspiration and courage, as well as keep you educated on the latest information on advanced melanoma.
Each body is different, and everybody reacts differently to each therapy. Advanced Melanoma is complicated. It is important to be educated about your options.
Your care team can provide resources on what to expect. However, the time it takes to experience progression cannot be easily predicted for each patient, and estimates vary depending on many factors such as the person being treated and the type of immune checkpoint inhibitor regimen used.
It is important to ask your care team about what to expect for your current and next treatment.
Building and connecting with your own community of support may give you inspiration and courage, as well as keep you educated on the latest information on advanced melanoma. Continue discussions with your doctor to learn about any new information.
There are many emotional points during a treatment path, and it’s important to communicate how you feel with your family and loved ones.
Building and connecting with your own community of support may give you inspiration and courage, as well as keep you educated on the latest information on advanced melanoma.
You are not alone. Guilt is a common feeling for people with advanced melanoma and can happen for many reasons. It’s important you take care of yourself and talk to your loved ones about your feelings.
If you feel you cannot talk openly about your feelings to those around you, counseling or support groups may be able to help you. Talk to your care team if you would like to find someone to talk to about your feelings.
Talk to your care team about feeling tired and ask if they can help.
Fatigue (tiredness) is a common symptom for people with advanced melanoma. It can lead to exhaustion. You may not be able to do the same activities you used to do. Even for patients who have been taking immunotherapy for years, fatigue can still interfere with everyday activities.
It is important to rest to help you feel less tired such as sitting or lying down.
Sometimes, even exercise can help with fatigue. You can try taking a walk, making more gentle movements in bed, or standing up.
Talk to your family and friends to help them understand that you are more tired than before.
It is important to stay educated and proactive in your care. You are the most important person in your care team.
Building and connecting with your own community of support may give you inspiration and courage, as well as keep you educated on the latest information on advanced melanoma.
NED and CR mean the same thing. They mean that the signs and symptoms of cancer are gone. However, some cancer cells may still be present at a very low level, meaning current tests cannot detect them.
PR stands for partial response, also called partial remission, which means the tumor(s) shrunk.
SD stands for stable disease, which means the tumor(s) did not grow and did not shrink.
Duration of response means the length of time that a patient has a response to treatment, meaning how long the treatment worked.
These terms basically mean side effects, or the signs/symptoms that you may experience while taking therapy. They describe how a medication affects your body.
As an advocate for your loved one, you may go to their appointments and should have a relationship with their care team. It’s important you help in getting accurate information about your loved one’s treatment path.
Ask questions when you have them. Stay educated and connected to the advanced melanoma community to know what to ask and what to expect.
Building and connecting with the advanced melanoma community of support can keep you educated on the latest information on advanced melanoma. There are also support groups just for caregivers of people with cancer.
Learn everything you can about advanced melanoma. Make sure to also learn about the specific stage and type of melanoma your loved one has. You can help get their medical records and even organize them.
Building and connecting with the advanced melanoma community of support, including reaching out to a doctor, can keep you educated on the latest information on advanced melanoma. There are also many organizations with resources dedicated to you: caregivers of people with cancer.
You are an important part of the care team.
When going to doctor appointments with your loved one, it’s important you help get clear and accurate information about the treatment path such as treatment options and what to expect. You can also help organize the information by taking notes during the appointment and asking questions.
Your role may change as the needs of your loved one change.
Talk to your loved one, family, and friends about your role to better understand the details of how involved you could be.
Building and connecting with the advanced melanoma community of support can keep you educated on the latest information on advanced melanoma. There are also many organizations with resources dedicated to you: caregivers of people with cancer.
It’s normal to feel overwhelmed and even unprepared. You are helping make decisions about medical care and taking care of someone. This can feel like a lot.
You may want to talk to your loved one, family members, and friends about what your role should be. Make sure to decide what your limits are and communicate them.
Delegating tasks and deciding how others can help is important: for example, shopping for groceries or taking care of the mail.
You need to take care of yourself, too. Plan things that you like to do. Ask for help. Try to eat healthy, exercise, and meet with friends. No one can do it all. No one can be a caregiver every hour of every day for months and months.
If things seem too overwhelming and feel like a constant problem, it’s important to talk to your own healthcare team to get professional help.
Carrying a notebook or having a device with you at medical appointments can help you jot down important details or questions you may have. You can also keep track of any side effects your loved one has when you are not at appointments.
If you are trying to send out updates or requests to a group of people, you may want to try an online tool to help schedule support.
Created in Partnership with the Replimune Patient Steering Committee
This site was inspired and formed by the insights of the Replimune Patient Steering Committee, a group of patients and caregivers impacted by advanced melanoma. These members are committed to sharing their perspectives and advancing the path ahead for others affected by advanced melanoma.


[empty]